Advancing Spiritual Care in Everyday Clinical Practice GWish Scholars

As part of the GWish Project, we are inviting our second cohort of clinician/chaplain pairs to develop and conduct demonstration projects consisting of interprofessional spiritual care clinical models that can be tested in multiple health settings.
BECOME A GWISH SCHOLAR
The purpose of these demonstration projects is to establish an evidence-base for spiritual care in clinical settings and share best practices among a growing network of spiritual care leaders through our ongoing Learning Collaborative.
As emerging leaders in this nascent field, all demonstration project participants will become part of a network of GWish Scholars, working with mentors, teachers, and fellow scholars to elevate spiritual health as a new standard of care across all healthcare systems.
If you or your organization wish to participate in this early-stage development of the field of spiritual health, we encourage you to apply. All teams must consist of one clinician and one chaplain from the same health setting.
The GWish Scholar demonstration projects have been made possible through generous funding from the John Templeton Foundation.
The GWish Scholar Demonstration Project Application is now closed

- Tending the Soul, Transforming Healthcare
-
ECMC Family Health Center, NY
Tending the Soul, Transforming Healthcare
Brent Anderson, MDiv, BCC
Sushama Thandla, MD
The setting for this demonstration project is the Erie County Medical Center's Family Health Center, an academic family medicine clinical setting for the Department of Family Medicine at the State University of New York at Buffalo. As part of the project, at least 200 patients will receive spiritual screening, to include spiritual history and a care plan if appropriate. Also, ongoing education on spiritual screening, history-taking, and referral processes will be provided for the clinical staff.
The project will identify facilitating factors and barriers to the effective implementation of standards for interprofessional spiritual care as recommended by GWish.

- Integrating Spriritual Care into Care Teams Serving High Risk Community Clinics
-
Baylor Scott and White Health, TX
Integrating Spiritual Care into Care Teams Serving High Risk Community Clinics
Daniel Roberts, MDiv, BCC
Jeffrey Zsohar, MD
The Baylor Scott and White Health team will fully integrate spiritual care in select Baylor Scott & White Community Care Clinics, to include spiritual struggle screenings, FICA spiritual histories performed by clinicians, and when appropriate SDAT (Spiritual Distress Assessment Tool) or PC-7 (Palliative Care 7 Assessment Tool) spiritual distress assessments completed by a professional chaplain. A spiritual care plan will follow, created by the chaplain and the care team.
This demonstration project will provide a blueprint for expanding spiritual care to outpatient clinics in healthcare systems throughout the United States.

- AHS Spiritual Collaborative Care Model
-
Atlantic Health System, NJ
AHS Spiritual Collaborative Care Model
Stephen Faller, MDiv
James Barr, MD
The AHS demonstration project team aims to build healthier communities by connecting patients, families, AHS physicians, AHS Chaplain services, and local resources through concrete and consistent spiritual care interventions.
In this demonstration project, outcome metrics will be aggregated and analyzed with a focus on patients with serious illnesses and/or chronic conditions. This will identify the impact of physicians and chaplains collaborating on screening, assessing, and implementing Spiritual Care plans.
Through this pilot, the AHS team hopes to improve patient outcomes and quality of life, while advancing interdisciplinary collaboration and job satisfaction among physicians.

- Integrating Spiritual Assessment in the Care of People with Primary Brain Tumor within an Outpatient Neuro Oncology Clinic
-
Mayo Clinic, FL
Integrating spiritual assessment in the care of people with primary brain tumor within an outpatient neuro Oncology Clinic
Beba Tata, MDiv, MPH, BCC
Kimberly Nelson, MSW, OSW-C
The purpose of this project is to demonstrate the impact of integrating spiritual care into the care of people with primary brain tumor using a generalist-specialist model. The neuro-oncology patient population was chosen because primary brain tumor is known to be a devastating disease with a bleak prognosis and detrimental effects on health-related quality of life.
This project will equip clinicians to identify the indicators of spiritual distress through screening and history taking and make appropriate referrals to chaplains for a comprehensive spiritual assessment.

- Spiritual Screening and Assessment of English and Spanish Speaking Patients in ICU Downgrade and ICU Recovery Clinic at UC San Diego Health
-
University of California San Diego Health, CA
Spiritual Screening and Assessment of English and Spanish Speaking Patients in ICU Downgrade and ICU Recovery Clinic at UC San Diego Health
Allison Kestenbaum, MA, BCC
Amy Bellinghausen, MD
The process of transitioning out of the ICU and readjusting to life at home at discharge is emotionally and spiritually challenging. Despite the pervasive nature of these spiritual concerns, there are no established procedures in the field for spiritual screening and assessment in this patient population.
The project team aims to demonstrate feasibility of a routine spiritual screening and chaplain referral workflow by ICU medical staff at the time of ICU downgrade and at first IRC visit, to include offering the described care to Spanish-speaking patients.

- Spiritual Screening and Assessment for BMT and Leukemia Patients to Address Unmet Palliative Needs
-
North Shore University Hospital (NY), Yasir Saleem, MA & An Gao Leung, MD
The project leverages the close collaboration between the GaP and Chaplaincy teams on the BMT and Leukemia floor to address the unmet palliative needs (including the spiritual domain) that patients with hematologic malignancies may have. This will be achieved by creating strategies to facilitate spiritual assessment (spiritual screening, history, and comprehensive chaplaincy assessment) as a standard of care and enhancing communication processes between the chaplaincy and palliative care teams.
This will be done by: 1) Process mapping, to improve workflow and define expectations; 2) creating a curriculum to educate palliative care providers on spiritual screening and the importance of a specialized assessment; 3) standardizing, enriching, and creating accessibility for documents related to generalist and specialist spiritual assessment; and 4) improving the way communication is achieved between the generalist-specialist dyad.
- What are the demonstration projects about?
-
The Advancing Spiritual Care initiative is requesting proposals for Demonstration Projects in the field of interprofessional spiritual care. These projects will be based on the Generalist-Specialist model of professional spiritual care, in which clinicians (generalists) collaborate with spiritual care specialists, such as board-certified chaplains. The goal of the current initiative is to support Demonstration Projects in spiritual assessment to include projects related to spiritual screening and history as completed by clinicians, and/or more comprehensive spiritual assessment as completed by chaplains. The Advancing Spiritual Care initiative is funded by The John Templeton Foundation; the project is led by PI Christina Puchalski, MD, of The George Washington University’s Institute for Spirituality and Health (GWish) in collaboration with Co-PI Kathleen Griffith, PhD, MPH, of The George Washington University School of Nursing, and Csaba Szilagyi, MDiv, MLA, MS, of Transforming Chaplaincy at Rush University.
The Generalist-Specialist model is fundamental to the practice of interprofessional spiritual care at GWish, and in the current Advancing Spiritual Care project. This model is the foundation of Demonstration Project design, and all proposed projects will be evaluated based on effective implementation strategies for Generalist-Specialist spiritual care in the focus areas of spiritual screening, history, and assessment as shown in the diagram below.
Figure 1. Inpatient Spiritual Care Implementation Model1
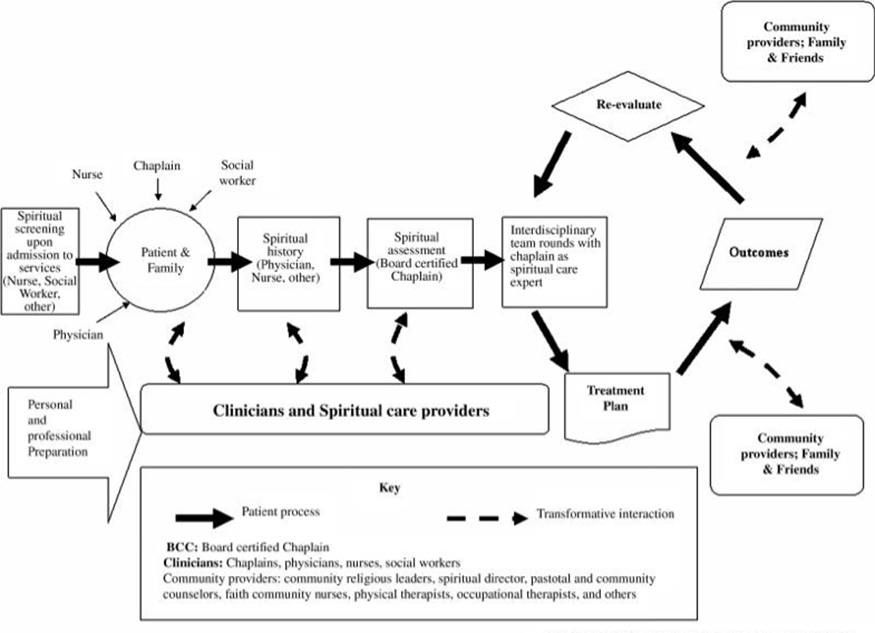
1Puchalski C, Ferrell B, Virani R, et al. Improving the quality of spiritual care as a dimension of palliative care: the report of the Consensus Conference. J Palliat Med. 2009;12(10):885-904.
This request for proposals (RFP) is intended to develop unique clinical models of interprofessional spiritual care through Demonstration Projects that can be tested in future research and practice to establish an evidence-base for spiritual care in clinical settings.
- What is the difference between demonstration projects and research projects?
-
While research expands new knowledge, demonstration projects (DPs) apply that knowledge in practical, immediate ways to improve care delivery on the ground. In healthcare, research and demonstration projects (or quality improvement projects) aim to enhance patient outcomes but differ in important ways. Research is designed to generate new, generalizable knowledge that can be applied beyond the specific setting in which it is conducted. It typically follows a structured methodology and requires ethical oversight, including Institutional Review Board (IRB) approval. Research studies often test hypotheses with the goal of contributing to the broader scientific understanding of healthcare practices or treatments. In contrast, DPs focus on improving specific processes or outcomes within a particular healthcare setting. It uses iterative, flexible methods and relies on real-time clinical or administrative data. DPs and research be conducted as pilot projects, which are smaller-scale projects that test or refine processes or interventions before larger projects are implemented.
Comparison of Features of Demonstration vs. Research Projects
Feature Demonstration Project Research Purpose Improve local care/processes Generate new, generalizable knowledge Generalizability Limited/local Yes Methodology Iterative, adaptive Rigid, controlled Data Source Real-time operational data Newly collected or existing data Example Reducing wait times in a clinic Clinical trial on new treatment Examples of Related Demonstration Projects Applied to Health Care Topics
Population Demonstration Project Homebound elderly patients Implement a process for RN spiritual distress screening and chaplain referral to increase frequency spiritual care and improve patient satisfaction with home care Women with late pregnancy loss Test a rapid referral process to chaplains for MDs and RNs on a post-partum unit for patients with late pregnancy loss to expedite establishment of spiritual care Family of ICU patients Develop and implement spiritual care multi-disciplinary rounds for clinicians and chaplains to ensure families of patients with prolonged stays receive ongoing spiritual care - How will the demonstration projects be structured and who should apply?
-
We will select five (5) US or global project teams composed of dyads of one clinician and one chaplain per team, from diverse clinical settings with a focus on spiritual assessment and implementation models of interprofessional spiritual care. Selected Demonstration Project clinician/chaplain pairs will be called GWish Scholars. The teams in this cycle will develop and implement Demonstration Projects in spiritual assessment that represent successful models of collaboration between clinicians and chaplains to build the knowledge and evidence for interprofessional spiritual care.
While the primary goal is to support implementation of the Demonstration Projects, we also recognize the opportunity to develop leaders in spiritual care, and thus selected GWish Scholar teams will participate in our Advancing Spiritual Care Learning Collaborative and structured mentoring of the project teams to share best practices and create a network of spiritual care leaders. From the project evaluation we hope to learn 1) the facilitating factors and barriers to effective implementation of existing guidelines and recommendations, and 2) the potential impacts of successful implementation of improved spiritual care on key stakeholders. This Learning Collaborative and evaluation process will inform future cycles of this initiative to create sustainable outcomes for establishing the field of spiritual care.
The Demonstration Projects in this cycle will focus on generalist-specialist spiritual care to include spiritual assessment (spiritual screening, history, and comprehensive chaplain assessment) and implementation models of interprofessional spiritual care. The primary goal of these projects is to focus on effective implementation of existing national guidelines for spiritual care. The National Consensus Project Clinical Practice Guidelines for Quality Palliative Care, and specifically the spiritual domain, serve as a key source to guide the projects (www.nationalcoalitionhpc.org). The NCP guidelines are based on the 2009 “Improving Quality Spiritual Care as a Domain of Palliative Care” national consensus conference1. The projects will aid in identification of facilitating factors and barriers to successful implementation of currently established recommendations, paving the way for improved implementation outcomes for spiritual care models.
- What do I need to know about preparing my proposal (application)?
-
Five (5) clinician-chaplain teams will develop and implement Demonstration Projects to be completed within two years. Each proposal should have a detailed and well-developed implementation plan and a precise evaluation plan. If the Demonstration Project team leaders do not have prior experience in research or QI projects and evaluation, they are encouraged to collaborate with a strong research mentor within their organization or obtain that expertise though the addition of a local or national research mentor, who will help ensure the project’s successful completion.
The proposal evaluation criteria include: 1) applicants’ CV and clinical background; 2) the Demonstration Project team and local mentors’ research or QI experience; 3) quality and feasibility of the proposed Demonstration Project; 4) commitment of the applicant’s organization based on the letters of support; 5) the potential for clinical implementation and assessment of potential impact for key stakeholders [healthcare system, patients, and clinicians]; 6) the potential for models that can be tested in future research or practice; and 7) a sustainability plan for future years.
- What are the requirements / expectations if I’m selected to participate?
-
During the two-year project development, implementation, and evaluation at their home institutions, Demonstration Project teams will be expected to:
- Participate in the initial virtual ISPEC course and virtual Demonstration Project Launch meeting
- Consult with the ASC Team to finalize their project plan and methodology before IRB submission
- Submit their project for approval by their institution’s IRB
- Participate in all virtual monthly Learning Collaborative sessions and session evaluation
- Participate in all scheduled mentoring calls with their Demonstration Project Advisor and Implementation Science Coach
- Conduct ongoing project evaluation
- Submit (1) article for publication and (1) abstract for presentation based on the ongoing or completed Demonstration Project
- Present Demonstration Projects at an ISPEC training
- Participate in the Final Demonstration Project Team Meeting
- Complete all Advancing Spiritual Care program evaluation and progress update/final reporting associated with participation in the two-year project
- Who is eligible to participate?
-
This cohort of Demonstration Projects is open to applicants in clinical settings within United States and globally. Each project should include a board-certified chaplain and clinician as project leaders. We realize not all settings have board-certified chaplains. We will consider applications with commensurate professional chaplaincy experience to include 8 or more years of clinical chaplaincy or 4 units of CPE and 2000 hours of clinical practice. “Clinicians” in all ASC activities include Medicine, Nursing, PAs, NPs, Social Work, Psychology, Physical Therapy, Occupational Therapy, and Speech Therapy.
- How much funding will be awarded to each project team?
-
Five (5) US or global projects will be funded through this initiative. Each Demonstration Project will receive funding of $100,000USD and the project duration is two years. Funds will be disbursed in (2) $50,000USD payments, the first in Year 1 and the second in Year 2.
- What costs are covered by the funding?
-
The funds from these awards for Demonstration Projects can be used for salary support of the project leaders (including salary and fringe benefits) and project staff, and other direct costs associated with the project such as consultant costs, statistical support or supplies. Travel and accommodations for the 2-day ISPEC/Final Demonstration Project Meeting to be held in Washington DC should be included in your budget. Indirect costs are not allowable.
- How do I apply?
-
The Advancing Spiritual Care Demonstration Project Application and instructions can be accessed via the link on this web page. Two webinars will be held July 16 & July 18 to answer questions about the application process. All applications are due 9/15/2025. Recipients will be notified by November 21. For questions regarding the Demonstration Projects, assistance in completing the application, or to RSVP for the informational webinars, please contact Cherron Gardner-Thomas at gwish [at] gwu [dot] edu (gwish[at]gwu[dot]edu).
- What rubric will be used to evaluate my application / proposal?
-
The following rubric will be used as a part of the evaluation process for DP applications/proposals. The rubric integrates evidence-based implementation science domains that are hallmarks/indicators of successful implementation outcomes.
Implementation Science Domains
Instructions: Please evaluate how well the application as a whole integrated and addressed each of the following implementation domains. See the definition of each implementation domain below.
Evaluation Rubric Scale
Scoring:
4=Excellent
3=Good
2=Limited, lacking details
1=Minimal
0=Not addressed at allAcceptability:
The perception of stakeholders that the demonstration project and the innovations, interventions, or practice changes to advance spiritual care are agreeable, palatable, high-quality, or satisfactory in the particular setting. It may entail stakeholders’ confidence in and satisfaction with project implementation and outcomes. Potential implementation stakeholders may include patients, clinicians/chaplains, administration, or health system.4- Proposal clearly describes the potential acceptability of the project and strategies to maximize acceptability among implementation stakeholders (e.g., patients, clinicians/chaplains, administration, or health system).
3- Proposal discusses the potential acceptability of the project
2- Proposal may mention the potential acceptability of the project but lacks details.
1- Proposal has a very vague or minimal description of the potential acceptability of the project.
0- Not addressed at all
Adoption:
The intention, initial decision, or action to try/employ an innovation or practice change proposed in the project and the stakeholder engagement or lack of engagement with the project throughout implementation.4- Proposal clearly describes how the project will facilitate adoption and engagement and address barriers and lack of engagement throughout the implementation process.
3- Proposal discusses strategies to facilitate the adoption of the project in the particular setting.
2- Proposal may mention adoption but lacks details.
1- Proposal has a very vague or minimal description of the adoption of the project.
0- Not addressed at all
Appropriateness:
Perceived fit, usefulness, suitability, or relevance of the proposed demonstration project with respect to the particular clinical setting and needs.4- Proposal provides a detailed description of the appropriateness of the project and why the project is a good fit for the particular setting.
3- Proposal discusses the appropriateness of the project and the fit for the particular setting.
2- Proposal may mention the appropriateness of the project but lacks details.
1- Proposal has a very vague or minimal description of the appropriateness of the project.
0- Not addressed at all
Feasibility:
The extent to which the demonstration project can be successfully carried out with available resources in the particular setting (e.g., personnel, money, time, infrastructure, communications, etc.). The degree to which the project is implementable and suitable/practical to implement in the setting.4- Proposal clearly describes the feasibility of the project and how it will be carried out with available resources.
3- Proposal discusses the feasibility of the project in the particular setting.
2- Proposal may mention the feasibility of the project but lacks details.
1- Proposal has a very vague or minimal description of the feasibility of the project.
0- Not addressed at all
Fidelity:
The extent to which the demonstration project will ensure that it is delivered as intended by the project team. The degree to which it will maintain high quality and adherence to the proposed plans for the innovations or practice changes to advance interprofessional spiritual care.4- Proposal clearly describes how fidelity will be achieved and maintained with regards to the project and explains how the project ensures that interprofessional spiritual care practice will be advanced as intended.
3- Proposal discusses strategies to ensure the fidelity of the project in the particular setting.
2- Proposal may mention the fidelity but lacks details.
1- Proposal has a very vague or minimal description of fidelity.
0- Not addressed at all.
Reach/Penetration:
The extent to which the project will reach the target audience/participants (e.g., patients, clinicians/chaplains, administration, or health system). The proportion of the target audience who are actually reached by the project in the particular setting. The degree to which the project outcomes/impact may potentially be adopted at the broader institution and beyond.4- Proposal clearly describes how the project will maximize its reach and penetration among target audience/participants and presents reasonable strategies to address barriers and opportunities.
3- Proposal discusses strategies to ensure the reach and penetration of the project in the particular setting.
2- Proposal may mention the reach and penetration of the project but lacks details.
1- Proposal has a very vague or minimal description of the reach and penetration of the project.
0- Not addressed at all.
Sustainability:
The extent to which the proposed demonstration project and the implemented interprofessional spiritual care practices continue after external grant support is terminated. The extent to which the new practices are continued, incorporated, integrated, or standardized in your setting resulting from the project.4- Proposal clearly describes the sustainability of the project and the potential for the implemented practices to be integrated and continue after grant support.
3- Proposal discusses strategies to ensure the sustainability of the project in the particular setting.
2- Proposal may mention the sustainability of the project but lacks details.
1- Proposal has a very vague or minimal description of the sustainability of the project.
0- Not addressed at all
Organizational Climate and Culture:
The degree to which the organizational climate and culture is conducive and supportive for the implementation of the demonstration project.4- Proposal clearly describes how the organizational climate and culture is conducive and supportive for project implementation.
3- Proposal discusses the potential organizational support for the project in the particular setting.
2- Proposal may mention the organizational climate and support but lacks details.
1- Proposal has a very vague or minimal description of the organizational climate and support for the project.
0- Not addressed at all
Leadership:
The leadership capability, experience, and potential of applicants for implementing the proposed demonstration project in their setting as reflected by the application as a whole.4- The application as a whole reflects a successful leadership history of implementing projects or a strong potential for leadership.
3- Proposal suggests sufficient leadership history and/or potential for project implementation.
2- Proposal may suggest leadership potential but lacks details.
1- Proposal has a very vague or minimal evidence for leadership potential. 0- Not addressed at allImplementation Science Domains were adapted from Proctor et al., 2011 (https://link.springer.com/article/10.1007/s10488-010-0319-7#Tab1) and Johns Hopkins Bloomberg School of Public Health (https://www.jhsph.edu/research/centers-and-institutes/global-mental-health/resource-materials/dissemination-and-implementation-science-measures/)
The GWish Scholar Demonstration Project Application is now closed
